Integumentary
System |
Introduction
• The skin covers the surface of the body and is formed
by the:
- Epithelial portion of ectodermal origin, the epidermis
- Connective portion of endodermal origin, the dermis
• Depending on the thickness of the epidermis, thick and
thin skin can be distinguished:
- Thick Skin: paw pads
- Thin skin: rest of the body, in some species the body is covered
by thick skin.
|
|

|
•
Below this and continuous to the dermis, we find the hypodermis
or subcutaneous cellular tissue that is not part of the skin, it
only serves to bind it to the subjacent organs.
- Hypodermis: loose connective tissue that can contain many adipocytes
that form the panniculus adiposus. |
Functions
• The skin is one of the largest organs with up to 16% of
the body weight and accomplishing uncountable functions:
- It protects the organism against water loss and abrasion thanks
to the stratum corneum of the epidermis
- It constantly receives information on the surrounding environment
and sends this to the CNS through sensitive nervous ends.
- It cooperates with the thermal regulation of the body through
blood vessels, glands and adipous tissue
- The melanin (pigment produced and accumulated in the epidermis)
protects against ultraviolet rays
- In the skin, vitamin D3 is formed by the sun’s ultraviolet
rays on the precursors synthesized in the organism.
>> The junction between the epidermis and dermis is irregular,
the dermis presents projections, the dermal papillae, that fit
in the incurvatures of the epidermis, increasing the cohesion
between these two layers.
|
|

|
Thin
skin |
 |
Thick
Skin |
|
| Epidermis
• Formed by keratinized stratified squamous epithelium
Cell types
Keratinocytes
• The most abundant, each cell that forms the epithelium
is a keratinocyte
Melanocytes
• Produce the melanin pigment
Langerhans cells
• Antigen-presenting cells, located throughout the entire
epidermis, between the keratinocytes.
Merkel’s cells
• Mechanoreceptors located in the deepest region of the
epidermis, supported by the basal lamina and bound to the keratinocytes
through the desmosomes
|
Layers
of the Epidermis (Thick skin) |
|

|
Stratum
Basale
• Formed by prismatic or cuboidal basophilic cells that rest
upon the basement membrane that separates the epidermis from the
dermis
• It is rich in epidermal stem-cells and is also called the
Germinal layer
• It presents intense mitotic activity and is responsible
along with the stratum spinosum for the constant renewal of the
epidermis.
• It
contains intermediate keratin filaments in its cytoplasm that become
more numerous as the cell advances towards the surface. |
|

|
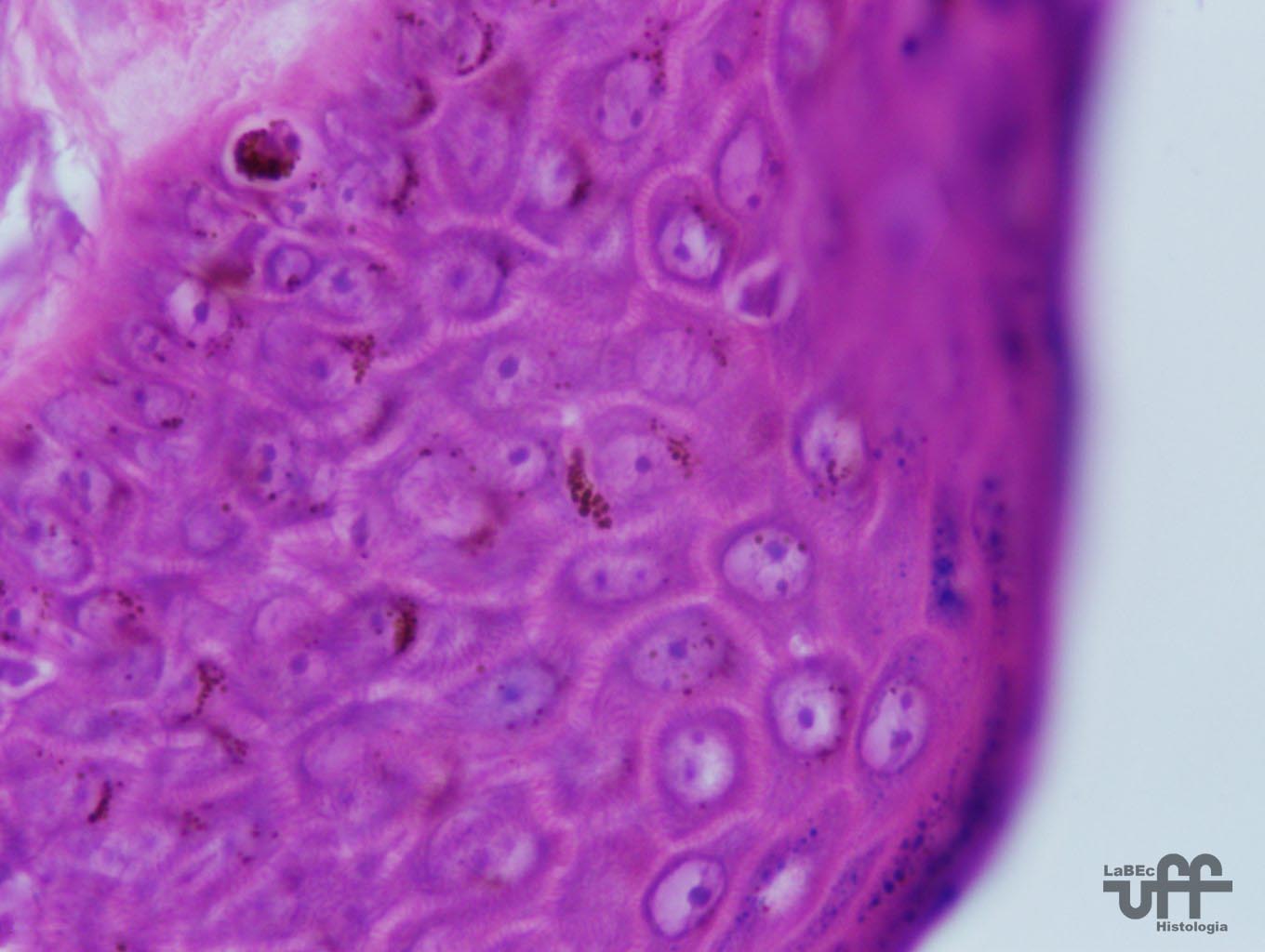
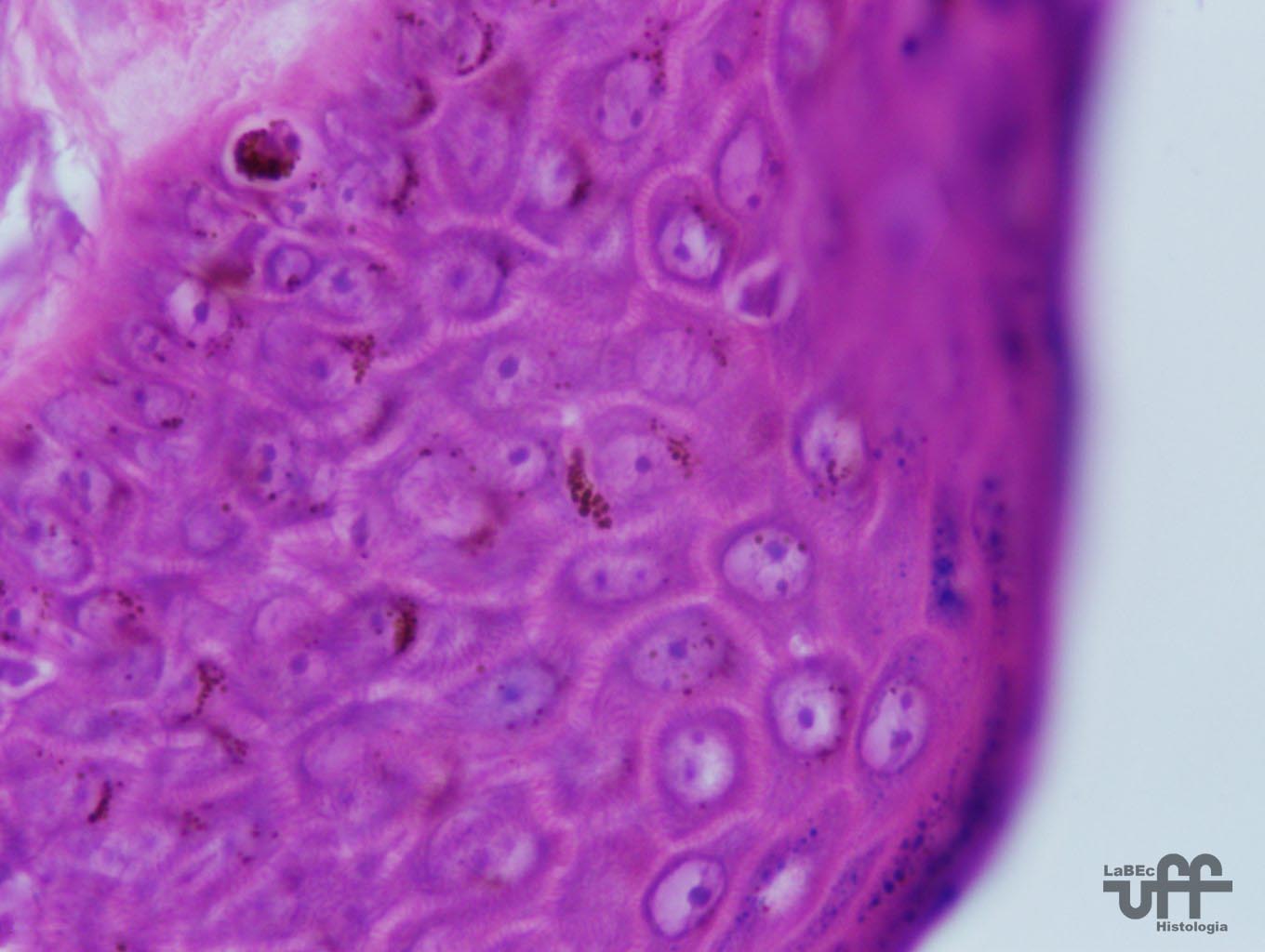
Stratum
Spinosum
• Formed by cuboidal or slightly squamous cells with a central
nucleus, a cytoplasm with short expansions that contain bundles
of keratin filaments(tonofilaments)
• The tonofilaments and desmosomes have an important role
in maintaining the cohesion between the cells of the epidermis and
in resisting abrasions.
• There are also keratinocyte stem-cells, and mitosis occurs
in the stratum basale and at a lower rate in the stratum spinosum. |
|

|
Stratum
Granulosum
• With only 3-5 lines of polygonal flattened cells with
a central nucleus and a cytoplasm rich in basophilic granules
called keratohyalin granules.
• The keratohyalin granules are not surrounded by a membrane
• They present lamellar granules, visualized only under
electronic microscopy, that contain lamellar discs formed by lipid
bilayers and are surrounded by a membrane. These granules fuse
themselves with the plasma membrane and release their contents
into the intercellular space of the granular layer, where the
lipid material is deposited and will contribute to the formation
of a barrier against the penetration of substances and turning
the skin impermeable to water and avoiding dehydration of the
organism.
• The waterproofing agent appeared in reptiles first and
is important under an evolutionary point of view so to allow life
outside the water.
Stratum
Lucidum
• The most evident layer of the thick skin, formed by a
thin layer of flattened, eosinophilic and translucid cells whose
nuclei and cytoplasmic organelles were digested by enzymes from
the lysosomes and disappeared.
• Its cytoplasm presents numerous compacted keratin filaments
and it is also possible to see desmosomes between the cells.
|

|
Stratum
Corneum
• It has a variable thickness, formed by flattened, dead
and nonnucleated cells
• The cytoplasm of these cells is filled with keratin
• The tonofilaments agglutinate along with the matrix formed
by the keratohyalin granules. At this stage of differentiation,
the keratinocytes are transformed into lifeless plates and continuously
shed.
|
Layers
of the Epidermis (Thin skin): the epidermis is simple,
frequently lacking the stratum granulosum and lucidum, and present
a much smaller stratum corneum.
|
Melanocytes
• The color of the skin results from various factors of
which the most important are: content of melanin and carotene,
and the amount of capillaries in the dermis and the color of the
blood in theses capillaries.
• They present a globular cytoplasm that originates extensions
that penetrate the incurvatures of cells of the stratum basale
and stratum spinosum and transfer melanin granules to the cells
of these strata.
• The melanocytes do not form demosomes with the keratinocytes,
but attach themselves to the basement membrane through hemidesmosomes.
• Once formed, the melanin granules migrate through the
extensions of the melanocytes and are injected through yet unclear
mechanisms into the cytoplasm of the keratinocytes that function
as deposits of melanin and contain a greater amount of this pigment
than the melanocytes.
• The melanin granules fuse with the lysosomes of the keratinocytes
and that is why the more superficial cells of the epidermis do
not contain melanin.
• In the epithelial cells the melanin granules are in a
supranuclear position, offering maximum protection to the DNA
against the hazardous effects of sun radiation.
• The genetic load influences the rate of activity of the
melanocytes since almost everyone has the same amount.
• The darkening of the skin due to solar exposition occurs
initially due to the darkening of the pre-existent melanin and
the acceleration of the melanin transference to the keratinocytes.
On a second stage, the synthesis of melanin is increased. |
|
•
Melanin is a dark-brown pigment produced by the melanocytes that
are found in the junction between the dermis and epidermis or
between the keratinocytes of the stratum basale of the epidermis.
|
| Dermis
• It is the connective tissue where the epidermis rests
upon, and that binds the skin to the subcutaneous tissue or hypodermis.
• The
dermis presents a varying thickness and its outer surface is irregular,
presenting saliencies, the dermal papillae, that accompany the
corresponding invaginations of the epidermis.
•
The papillae increase the contact area of the dermis with the
epidermis strengthening the link between these two layers, the
papillae are most frequently found in the zones subject to aggressions
and abrasions.
•
The dermis is composed by two layers with slightly distinct limits
: The superficial Papillary Dermis and the deeper Reticular Dermis.
• The papillary layer is thin, composed of loose connective
tissue that forms the dermal papillae. In this layer, special
collagen fibrils were described, that insert themselves on one
side into the basement membrane and on the other side penetrate
deeply into the dermis, forming the dense connective tissue.
• The reticular layer is thick, composed of dense connective
tissue.
• Both layers contain many fibers of the elastic system,
partly responsible for the elasticity of the skin.
• Asides the blood and lymph vessels, and the nerves, the
following structures derived from the epidermis are found in the
dermis: hair follicles, sebaceous glands and sweat glands.
|
| Sensory
receptors of the Skin
Pacinian
Corpuscles
• They capture special vibratory and tactile stimuli
• They are formed by a nervous fiber whose unmyelinated
end portion is surrounded by many layers that correspond to various
supporting cells.
• The end-layer is capable of sensing the application of
pressure, which is transmitted to the other layers and sent to
the corresponding nervous centers.
Merkel
Discs
• They detect specially pressure and tactile sensibility.
• An afferent fiber is normally branched with many end-discs
of this kind of nervous branching.
• These discs are comprised in a specialized cell whose
distal surface is fixed on epidermal cells through an extension
of its protoplasma.
• This way the movements of pressure and traction on the
epidermis result in a stimulus.
Free
Nerve Ends
• Sensitive to mechanical, thermal and specially pain stimuli
• Formed by a branched axon surrounded by Schwann cells,
and these are both surrounded by a basement membrane.
>>
Glabrous (hairless) skin exclusive receptors
Meissner’s
Corpuscles
• Sensitive to touch stimuli
• They are in the hairless saliencies of the skin.
• Formed by a myelinic axon whose end-branches are entwined
with accessory cells.
Krause
End-Bulbs
• Cold-sensing thermal receptors
• They are formed by a nervous fiber whose ends have a club
shape.
• They are placed in the boundary region of the skin and
mucous membranes ( e.g.: around the lips and genitals)
SURFACE
RECEPTORS |
SENSATION
PERCEIVED |
Krause
receptors |
Cold |
Ruffini
receptors |
Heat
|
Merkel
discs |
Touch
and pressure |
| Vater-Pacini
receptors |
Pressure |
Meissner
receptors |
Touch |
| Free
nervous ends |
Mainly
pain |
|
Hairs
• The hair follicle has a terminal dilation , the Hair Bulb,
that contains the Dermal Papilla
• Covering the Dermal Papilla are the cells that form the
root of the hair.
• The central cells of the hair root:
- Produce large, vacuolized and poorly keratinized cells that form
the Hair Medulla
- Following this and in a lateral position, the cells that originate
the Hair Cortex are seen.
- More peripheral epithelial cells originate the internal and external
sheaths.
- External Sheath: continuous with the epithelium of the epidermis
- Internal Sheath: disappears once it reaches the region where the
sebaceous glands release their products.
• Between the Hair follicle and the connective tissue around
it is the Glassy Membrane.
• The connective tissue that surrounds the follicle is thicker
and forms the Connective Sheath of the Hair Follicle
• Each one is an independent gland(compound alveolar tubule)
• Stretched out obliquely and inserted on one side in the
Connective Sheath of the Hair Follicle and on the other in the Papillary
Layer of the Dermis are the arrector pili muscles, whose contractions
pulls the hair into a more vertical position, bristling it.
• The presence of melanocytes gives the hair its coloring
and they are placed between the papilla and the epithelium of the
hair root, and provide melanin to the cells of the hair root and
cortex.
|
|

|
Hair
Follicle |
 |
Hair
Trio |
|
Hair
Trio
• Formed by the Hair Follicle, the arrector pili muscle and
the sebaceous gland. |

|
Sebaceous
Gland
•
Placed in the Dermis and its ducts generally open in the Hair
Follicle
• However, in certain areas( lips, glans penis and labia
minora of the vagina) the ducts open directly onto the surface
of the skin. The glabrous skin of the palms and soles do not have
sebaceous glands.
• The sebaceous glands are alveolar and generally a series
of alveoli debouch into a short duct.
• The alveoli are formed by an outer layer of squamous epithelial
cells that rest upon a basement membrane. These cells proliferate
and differentiate into round cells that accumulate in their cytoplasm
their secreting product of lipid nature.
• The nuclei gradually condense and disappear. The more
central cells of the alveolus die and disintegrate, forming a
sebaceous product.
• The sebaceous gland is an example of a holocrine gland,
since its secretion results from the death of cells. |
|

|
Sweat
Gland
• The merocrine sweat glands are very numerous and throughout
the skin, except in certain regions such as the glans penis.
• They are simple coiled tubular glands whose ducts open
at the surface of the skin.
• The secreting portion is found in the dermis, the secreting
cells are pyramidal and between them and the basement membrane
are the myoepithelial cells that help release its secretion.
•
The duct of the gland opens at the surface of the skin and follows
a helical course as it crosses the epidermis.
• It is formed by stratified cuboidal epithelium(two layers
of cells) that rest on a basement membrane.
|

|